Electronic medical records (EMR) data visualization
Just half of century ago, patient records in the medical practice were kept in the form of traditional written / typed documents. One of the most important developments in the medical practice that was possible with the technological enhancement of computers and, later on, the internet, is considered to be the electronic medical record (EMR). Not only did it permit a better and easier management of patient information within the healthcare unit, but is also made possible the integration of patient intelligence at local or even national level, this integration being vital in the perspective of treating or moving the same patient to other hospitals.
The patient record arose in the 19th century as a highly personalized ‘lab notebook‘ that clinicians would use to record their observations and plans so that they could be reminded of pertinent details when they would next see that same patient (Shortliffe, 1999).
In 1994, Edward Tufte, one of the most respected authorities in the field of data visualization, predicted that ‘medical records will soon be computerized‘, which will overcome the disadvantages of handwritten of printed documents. He best described the traditional, written medical record with the acronym WORN (write once read never), by contrast with the acronyms WYSIWYG (what you see is what you get) and WORM (write once read many) (Powsner and Tufte, 1994).
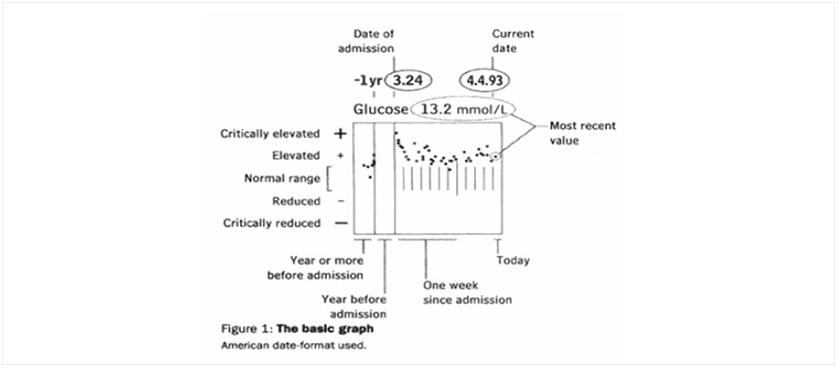
The authors further on suggest a graphical summary of patient status that illustrates the course of an illness and the treatment outcomes for a patient under examination. Both previous patient data and most recent results are included and complex clinical relations can be shown in order to test hypothesis. The graphics are supported by commercially available software and hardware and were created by extracting information from the traditional patient record and introducing it into the software used. As the authors finally put it, instead of a 5 cm thick record, a single page reveals the patient status graphically.
In 1999, Edward Shortliffe argued that, at that point, ‘no clinical computing topic is gaining more attention than electronic medical records‘. He then described electronic patient record as the ‘medical record in a new incarnation: electronic, accessible, confidential, secure, acceptable to clinicians and patients, and integrated with other, non-patient-specific information‘ (Shortliffe, 1999).
He took the discussion further and described the concept of integrated clinical workstation, representing a single entry point into a medical facility in which computational tools not only assist with clinical matters (results reporting, order entry etc.), but also with administrative work (Admission-Discharge-Transfer process, materials management, payroll), research (quality assurance, clinical trials) and scholarly information (digital libraries, drug information databases etc.).
While the electronic medical record would be at the heart of this integrated clinical workstation, the author argues that it would represent not an object in itself, but rather a set of processes that involve automation, such as processes for data collection and integration from various sources, as well as tools for displaying the data, analysis and sharing (Shortliffe, 1999).
Along with the complexity of systems and processes EMRs require, another issue associated with the electronic patient records is the security and confidentiality of patient information. However, considering the results of s study conducted in U.S. in 2009, it seems that it is not a matter of patients’ security concerns (as in electronic banking and ecommerce, if benefits are high and security guarantees the same, people will finally resort to it), but rather a matter of hospital and doctor choice or possibility. The study revealed that less than 2 percent of U.S. hospitals have adopted fully functional electronic medical records, most citing the required costs as being the biggest barrier (Steenhuysen, 2009).
References:
- Powsner, S., M. and Tufte, E. (1999), Graphical summary of patient status, The Lancet, Vol. 344, pp. 386-389
- Shortliffe, E., H. (1999), The Evolution of Electronic Medical Records, Academic Medicine, Vol. 74 No. 4 , pp. 414-419
- Steenhuysen, J. (2009), Few U.S. hospitals have electronic medical records
Image Source:
Powsner and Tufte (1994)

Tags: Data Visualization, Healthcare performance